Wessex
 Faculty
Faculty
The 20th George Swift Lecture
Delivered in Winchester Guildhall on the evening of 16th October, 2001 by Dr James Willis
Listen to the Juggler
General practice is a juggling act, it’s about keeping a seemingly-impossible number of balls in the air. A generation ago we used to add our own balls to develop our act. Now there has been a radical change, and other people add them for us. I am going to argue that if you want to know how this new arrangement is working, you don’t listen to the people adding the balls - you listen to the juggler.
Ladies and Gentlemen, if there is any task in life more challenging than trying to be a good GP, it is the task of getting your voice heard in high places whilst remaining ‘just’ a GP. I am therefore deeply grateful for the honour which the Wessex Faculty of the Royal College of General Practitioners has done me in asking me to give this twentieth George Swift lecture. And for this opportunity to say, or try to say, something which seems to me of great importance from my experience of juggling away, with so many of you here, for more than thirty years on the front line.
Thank you for coming to listen to me, every one of you.
Opportunity
?There are a number of us here who heard George Swift give the first of these, his own lectures, in 1981, and this was the final point he made, addressed to new entrants to general practice:
"I say the future is in your hands. You will all have an opportunity to do something new or original. Watch for your opportunity and make it when it comes."
Not all societies, however, have fostered individual opportunity. And if we think it is important to continue this for our society, and for the new generation of young doctors, I think we’ve got a fight on our hands.
Giants walked the earth in those days
My career in general practice began, as it now ends, with George Swift. It was in 1968 that I wrote to him asking whether I could join his Wessex GP Training Scheme. I was in the second year of a series of house-jobs in London and I wanted to know whether I could just come in for the last year of his rotation to pick up the ‘minor’ specialties, as we called them in those gloriously non-politically correct days.
It is important for my story to make it clear that I thought George Swift would, shall we say, jump at the chance to have me.
Harry Levitt
I had trained at the Middlesex Hospital, London, which had been his medical school 25 years before. And there I had been electrified – not too strong a word – by a little series of talks given by another of his great contemporaries in general practice, Harry Levitt.
Those sessions, which only a few of us attended, comprised the only exposure to general practice deemed appropriate in the entire course at The Middlesex, which prided itself on the small proportion of its students who ‘ended up’ in general practice.
But Harry Levitt’s quiet description of his work showed me a human kind of medicine which I found utterly different from, and infinitely more appealing than, the forbidding, steely-cold machinery of specialist medicine. So I went ahead and contacted Harry Levitt and arranged my student-elective in general practice.
David Morrell
Through him I visited a number of pioneering practices around the country. Including the first and then the only university department of general practice, Professor Richard Scott’s in Edinburgh. There I spent most of my time with a young doctor named David Morrell. Again, I was inspired by the human warmth I witnessed in consultations and, especially, in home visits.
(Years later, when David Morrell had become Professor of General Practice at St Thomas’ and then President of the British Medical Association,
I contacted him about a little difficulty I was having getting approval for extended study leave. He summed my problem up at once: "They’ll want you to measure something…")
Anyway, one of the things that most struck me about this student experience, in contrast to hospital medicine, was that ALL the GPs I met loved their work. From then on I was the student at the Middlesex who wanted to be a GP. There were no others in my year, and none that I knew of in the year above, or the year below. I was also probably the only person in the hospital who had any real experience of general practice. Not that that stopped most having disparaging opinions…
John Nabarro
But not all… Qualifying at the Middlesex with what was seen as this humble ambition (at one job interview I was asked whether I thought general practice had any future) I suddenly found myself the stunned occupant of the most academic, prestigious and demanding house-job in the hospital (With no official time off, night or day, for six months. Not to mention no acknowledgement of the fact I was married).
I was ‘Nab’s Houseman’. John Nabarro (later Sir John) was one of the great doctors of his generation. Part of that greatness was undoubtedly the fact that he used sometimes to refer to GP’s as, ‘proper doctors’.
And I think he did mean, ‘doctors who ‘juggle’ the whole of life.’
Anyway, after all that, here is George Swift writing back to me to say that I couldn’t just come in for the second year of his rotation, it would have to be the whole thing or nothing. I didn’t want to do Obstetrics again, I’d already got my Diploma, and I was sitting my Diploma of Child Health, after another highly sought-after house-job at the Whittington, so that was that. I went straight ahead with applying for Trainee vacancies.
Tony Danby
Which brought me to Wessex. To Lyndhurst, where my trainer was Tony Danby. Who, previous experience notwithstanding, was the best doctor, the most proper doctor, I have ever known. And who remains, as I suppose is appropriate for a trainer, my model.
During that happy year, living in a little cottage which grew gifts of vegetables on its doorstep, I saw George Swift every Wednesday at the day-release course which he ran with Philip Carter in Winchester and Southampton.
George Swift
I, and I think most of the trainees, found George Swift a difficult person to know. He certainly didn’t parade his distinction, and I admire the fact that he didn’t need to. He spoke briefly in introducing and concluding sessions, and almost never expressed a personal opinion. - This was in contrast to the rest of us - I remember my later surprise at the candour of an aside in, I think, his William Pickles lecture, when he referred to, "the myth that doctors are too busy to do anything.".
His somewhat dilapidated, gruff, appearance on the course, glimpsed through his tobacco smoke and wracked by his famous cough, was, I have often thought, a monument to the futility of health education.
And yet education was his baby. Returning from the war after distinguished service in the Royal Army Medical corps he had joined a practice which was both traditional, with separate entrances for private and panel patients, and advanced, with purpose built premises and attached nurses. He immediately moved to fill the postgraduate vacuum, founding the EC1 club in Winchester and Southampton, then being invited by John Hunt to join the Foundation Council of the Royal College of General Practitioners, because it had ‘similar objectives’. He was elected chairman in 1967. With John Revans and Ian MacDougal he pioneered Health Visitor attachments to practices and created the first GP vocational training scheme in the world, Chris Brill was the first trainee, and Philip Carter the second. Both are here tonight. He was the first and for a while the only Regional Adviser in General practice, and so on, and so on…
George Swift was a central figure amongst the extraordinarily highly-motivated group of great men and women who set about raising General Practice to its proper status in the eyes of the world, and who succeeded to an extent which is now far-too-easily taken for granted.
Hopeful travellers
Giants walked the earth in those days. And this is the point I am bringing out : the modernisation of general practice was brought about by individuals. Real people. Eccentrics. Driven by their own internal motivation. General practice was a wilderness and a challenge to anyone who wanted to make a personal mark and change things for the better.
The irony is that the change brought about by George Swift’s generation set in train the very processes which now threaten to remove the free and challenging environment which provided their own motivation. When I talk to people who knew George Swift well, and who hold him in the most genuine affection and admiration, I ask them whether they think he would have approved of the current situation. And the answer is a, "No" – with a "He would have been appalled" or a "He would certainly been disappointed and concerned" according to generation.
So there is a Paradox if you like: George Swift, as much as anyone, was the father of GP training, but if there was ever a doctor you can imagine resisting compulsory training for himself it was George Swift. I am glad I didn’t try to tell him to use a critical incident audit pack. Still less tell him to report back.
There is even a document written by him which says "I rather wonder now whether, if I were a young doctor, I would be as inclined to join the college." This document is undated, but he told Philip Carter without any great enthusiasm that he, Philip, really ought to take the MRCGP examination if he was going to teach. But one senses that he was less sympathetic with the college’s growing regulatory role than he was with its original educational aims.
You could almost say we have reached a reductio ad absurdum of the causes George Swift originally espoused. Good causes, they have just been taken too far.
It is said that it is better to travel hopefully than to arrive. George Swift travelled hopefully - perhaps we have arrived.
25 years on - My experience
I travelled hopefully as well. I belong to the generation which enjoyed the benefits of the wave of new-found self-confidence in general practice. It was an enormously exciting time and we had no doubt that we were embarking on the best job in the world. Drop-outs after training were unheard of – we all chose our practices and went straight in, bargaining to become principles as quickly as possible.
General practice in the 1970s and 80s was a ferment of innovation. I threw myself at the challenge as much as anyone. I used to tidy and summarise notes between patients (in the days when we sometimes saw forty in a surgery), my wife and I sat in the evenings when the children were asleep writing out age-sex register cards. We used various methods of analysing morbidity (as I had seen Harry Levitt using his E-book in his single handed practice in North London). I invented systems of organising chronic visits, starting with edge-punched cards and moving on to programs I wrote in BASIC. For computers such as the Commodore PET which I bought with a year’s trainer’s grant (£2,500, complete its double floppy-disc drive!). I published papers in the BMJ on my chronic visiting system and its accompanying dependency assessment scoring system, visiting all of my over-75 year old patients in order to do so. At the instigation of the nurses in our treatment room who wanted us to Do Screening I wrote a self-administered Health Screening program which was used by two and a half thousand of our patients, and which numerous other practices, including one in Pakistan, used as well, and which won me the 1989 John Perry Prize of the British Computer Society. I wrote my own programs to organise everything from Diabetic Clinics to Fun Runs. And clearing out my files two weeks ago I found a letter dating from the mid-eighties regretting that my then partner, Sheila Cassidy and I couldn’t participate in a particular research project because we had nine on the go already, and I had just been selected for an intensive study of my work which involved making a record of what I was doing every half-hour.
Internal motivation
Nor was this story unusual. And it was all entirely self-motivated, nobody told us to do ANYTHING.
When the Benzodiazepine group of hypnotic and sedative drugs appeared, for example, with their enormously increased safety profile in comparison to the then extraordinarily-widely consumed Barbiturates, GPs all over the country, following the example of doctors in Ipswich as it happens, set about the huge task of changing their patients to the safer drugs or weaning them off altogether. In a relatively short space of time the job was done, flexibly and sensitively, without any central direction whatsoever. Just personal example, peer-pressure and professional self-respect.
The administrative cost was NIL.
A very fundamental mistake
But from very early on I became worried by the direction the college was taking. In 1979, at the time of its 25th anniversary, I submitted an article expressing my fears to the British Medical Journal, which I thought was more widely-read than the College Journal. It was published as a Personal View, my first-ever publication.
I said that I thought the college was becoming inward-looking and bureaucratic, and that it was increasingly concerned with erecting hurdles for young doctors. It was trying to advance the status of general practice, and the status of its senior members, who had themselves joined it as a club, by making general practice more like a speciality. It seemed to me that the college was undermining the very things that made general practice special. It was adopting ceremonial, gowns, maces, entry examinations, just like the stuffy specialities that had so repelled me.
This mattered because it was symbolic of an attempt to make general practice exclusive whereas the true nature of general practice is inclusive. I felt, as I still feel, that this mistake was very fundamental indeed. As I expressed it better on a later occasion, the college was trying to describe general practice in a language which denied its very nature.
I was shy in those days, I didn’t expect my article to be published, and when it was published, I expected what I said, if it was noticed at all, would be loftily dismissed.
In fact what happened was that the Chairman of Council of the College, Ekke von Kuenssberg, invited me out to dinner.
We walked together to a nice little restaurant in South Kensington, and I discovered something about the college which I know still applies, it contains a rich variety of people with widely different views and it is eager for new input and new ideas. Kuenssberg listened to what I had to say, made some points of his own, and most important to me, told me to ‘keep writing’.
There was quite a gap, but I have done my best…
50 Years on – The new generation
So that’s George Swift starting in practice, and me starting, roughly 25 years later. What of young doctors starting now, after another 25 years, with the college on the eve of its 50th anniversary? What is the prospect for them?
Now, we all know the danger of looking at the past with rose-tinted spectacles. John Donne put it bluntly:
‘I have not been so pitifully tired with any vanity as with silly old men's exclaiming against our times and extolling their own'
But I’m going to risk being thought a silly old man and say that something has changed, and that one of the symptoms of the change is the lack of enthusiasm and whole-hearted commitment on the part of many, though mercifully not all, young entrants to general practice today.
la crème de la crème…
Teaching has always been an important part of medicine. Doctor of course means ‘teacher’. We have close affinities with the teaching profession. Particularly me, married as I am to a ‘proper’ teacher.
I taught medical students for most of my career in their first, third and fifth years. I became a trainer and then (returning full circle) an organiser, with Cled Jenkins, on my own, old Day release course, here in Winchester, during the late 1980s.
In that second half of the 1980s we could fairly say that we were getting ‘la crème de la crème’ of the Nation’s youth. It is a fact that Medicine was then the most difficult university subject to get into and general practice was by far the most popular career choice within medicine. I found Wednesdays wonderfully stimulating, Migrinogenic, but immensely worthwhile, in the company of these young doctors.
Once again, we organisers were left entirely to our own devices, there was no outside direction that I was conscious of. Vocational training itself had only become compulsory in 1981 (barring the route by which almost every outstanding GP I knew of, including Tony Danby and George Swift of course, but also a number of my contemporaries, had entered practice), there was no summative assessment for the trainees and they didn’t have to take the MRCGP, although if they failed it (after surmounting so many other obstacles and with eight years of experience) it was more a criticism of the examination than of them.
…treated like galley slaves
Today, general practice is to a large extent run by that generation of superlative doctors, and we see them being treated like galley slaves, audited, spied on, criticised, stereotyped, distrusted. Expected to comply with an impossible agenda set by other people. We see them being asked to juggle other people’s balls. Other people who chose easier routes in life, or who didn’t have the balls to stick the real job.
1990
It was in 1990 that the darkness came.
Use that phrase and a whole generation of doctors knows at once what you mean. We had seen it happen to our patients in other areas of life, and particularly we had seen it happen to teachers, but now it happened to us. We were modernised, brought to heel. The system wasn’t ‘broke’, far from it, but it was different, so they fixed it anyway.
Successive Labour governments had resisted the temptation to use the fact that they paid the doctors to justify calling the medical tune. I really believe they understood the danger. Margaret Thatcher, on the other hand, although she bitterly opposed Socialism, used this Achilles heel of the medical profession which was exposed to her by ‘Socialised Medicine’. It was as though she did not recognise doctors as being real people who needed to be given their heads like everybody else. Perhaps because of her instinctive disdain for the public servants we were proud to be.
I said at the time, "If this is a government that believes in freedom, Heaven help us if we ever get one that does not!" Well, that’s more or less what happened. Having always regarded myself as a radical idealist I suddenly found myself being described by Tony Blair, of all people, as a, "Force of conservatism … holding the nation back". It was another dark time.
Overall responsibility
The 1990 contract had actually been easier. I simply didn’t comply with it. Because I believed that it was incompatible with my responsibilities to my patients, on whose behalf the government was acting as an agent to employ me. A doctor cannot serve two masters. This is a thesis which has been elaborated since by myself and others and, in as far as there has been any argument at a higher level than the ‘do it or else’, level, I have no doubt we have won it.
At the time, and this is where we return to the juggling image, I wrote to the Health Authority telling them that my time was already full and that before I started doing the now-compulsory three-yearly height checks on ever adult, for example, and drawing the inevitably dull graphs, I wanted them to tell me what to stop doing in order to make time for this activity. Choosing what to stop doing, I explained, reflected my overall responsibility. That was the difficult bit, the bit which justified the respect in which my patients held me. The authority replied that they couldn’t tell me what to stop doing, so I said, ‘fine’, wrote the whole thing up in my shiny new annual report, probably even now on file in a dusty archive, to be eternally unread, and that was the end of the matter.
The most important case for treatment
But ten years on from then it isn’t so easy. They’ve got me and I know it. I am not going to bore you or depress you with the list of agencies lining up to control me now, to check on my re-education, to go through a show of pretending to make sure I am not a Harold Shipman, (even the police took years and they knew what they were looking for) there is a list of the agencies on my website (a little diversion if you like) incomplete, of course, it’s hard to keep up, but nonetheless impressive. There is even a regulator of doctors’ regulatory bodies.
In Sir Ian Gilmour’s words, from his diary of the Thatcher years, "Dancing with Dogma";
"Characteristically, however, devotion to the free market was combined with the imposition of unprecedented and ill-judged central controls on the daily work and priorities of individual doctors."
Dancing with Dogma – Britain under Thatcherism. Page 156
Believe me, you’re paying for all these people, go and have a look.
Once again I am opposed to this change on principle, and this time I have had to leave. I want you to know this, because the very real power of the individual doing something on principle is lost if nobody knows about it. The most enthusiastic GP of all, who inspired colleagues, students and young doctors, yes, I did, is leaving early, on principle, because he believes that the madness of the modern world is now the most important disease that he as a doctor ought to be trying to treat.
The patients understand, almost without exception. I have been telling some of them about this lecture that I am giving just after my retirement.
"Yes, we’ve lost the plot", said a hard-pressed plant-hire operator, in one of my last surgeries. Salt-of-the-earth type, father of three of ‘my babies’, all now in their teens. "We’ve lost the plot",
And another, a lady who lost her husband when I arrived nearly thirty years ago and has aged at what must be the same rate as me since then, "Why can't they let the people who know their job get on with their job?"
"Yes, that is exactly what I am going to talk about. I tell you what – I’ll quote you."
"Why can't they let the people who know their job get on with their job?"
The dominant position occupied by the executive tier of our advanced, democratic society ought to be one of its most-discussed anomalies.
If these people wanted to be doctors, they should have trained to be doctors. Surely they ought to be there to enable, and to keep control to a minimum, especially when things are running well. But we all seem to have swallowed the line that progress necessitates regulation and audit by the centre. Only brave souls directly challenge the mantra of accountability.
Accountability and medicine
Although doctors did not create the current situation, insofar as they acknowledge and participate in the ideology of accountability they are colluding in its perpetuation.
Journal of the Royal College of Physicians January 1999
Bruce Charlton, who wrote this, last year publicly declared his own refusal to co-operate with the QAA (Quality Assurance Authority) inspection of his academic department in Newcastle. Nothing happened, the inspectorate, wisely, ducked a confrontation with such a formidable thinker. They are not used to having to justify their activities, any more than NICE, or any of the other agencies being set up to control doctors are. They all take their legitimacy for granted.
Certainly the press and the legal profession take it for granted that people doing important things like medicine and teaching must, in the Brave New World, be controlled from the centre. Although, predictably, neither group thinks this is necessary for themselves. But for doctors, they think the more that is defined and controlled by protocols and rules, the better.
You can’t be too careful.
You’ve got to be ‘covered’
And we do collude in this ideology. Our college, certainly, has colluded with it. We do think it is necessary – or rather - our heads tell us it is necessary while our hearts disagree. We are like slaves who acquiesce in our slavery because we have been told that it is the only way the world can work.
An untested drug
But nobody knows whether it will work. In the history of civilisation it is a very new idea. As we have said, it would have been unthinkable to George Swift, and it was unthinkable to me for most of my career.
Now, the government professes its subservience to ‘Evidence’. Yet this radical new way of running the world, and now medicine, in detail from the centre has never been tested, and is certainly not evidence-based. No-one is looking for unwanted effects, but my patients and I can see them popping up all over the place. They may not be visible from on high, that is my central point again, but down here they increasingly dominate our lives. Down here, we are inclined to think that for all the imperfections of medicine when it was run by doctors, medicine run by spin-doctors, with their eyes focussed on the next election, is a great deal worse.
It’s not that ‘they’, the executive, are not intelligent. I know that the junior health minister, Yvette Cooper, for example, is very intelligent, and not because I have seen IQ tests or performance indicators which say so. I know for a much better reason than that; my wife taught her Biology for a number of years and has always said she was one of the brightest pupils she ever taught.
Virtual reality
These clever people get it wrong. As I have examined in detail in my books, the view from on high contains immensely powerful distortions and illusions, which are hidden by the very power of the tools which produce them – information technology, mathematical models, selective reporting, and so on.
These tools give a very strange, selected view of the world, producing a virtual world which seems more real, more valid, than the real thing. This is because there is no handle available by which they, or indeed any of us, can get a fix on the scale of the distortion. We read about a single sensational case and we are simply not equipped by nature to keep it in proportion with the rest of life.
The Inverse Scare Law
Thus we get what we might call the Inverse Scare Law, the more unlikely a danger is, the more we worry about it. And unless we tackle the problem at root, by confronting the illusion and educating ourselves about it, there will be no end to this. However safe we make the world, people will continue to worry about the remaining problems. And history tells us that they will worry even more about them.
And there will be remaining problems. Measured on the parameter of saving lives, general practice has an ultimate success rate of zero. Now I know you know this, and our patients certainly know this, but the people who now presume to control us often appear to have forgotten it, and so much else.
Trying to bridge the gulf
Stand back far enough from life and it seems that nothing is safe and nobody can be trusted. This is the opposite of most people’s first-hand experience.
That is the difference. That is the gulf I am trying to bridge. If you take on the task of legislating to abolish the endless store of rare events which the media selects to feed its public’s appetite for sensation you will bring daily life to a halt. You will swamp real people with protocols and paperwork which seem, on the ground, like utter madness. I have suggested that the quest for the abolition of Risk from life, the Utopian Illusion, is the great doomed quest of our age, analogous to the search for the Holy Grail, the Philosopher’s Stone, and scientific proof of the existence of God.
A matter of life (and death)
The qualities of single-mindedness and focus which are so prized on high are of little use to the GP, or to the teacher, trying to do the real job, the whole job, on low. The super-clever executive is like Douglas Adams’ Marvin the robot,
"Look at me. I’ve got a brain the size of a planet, and they tell me to go and look at flesh-eating bugs in Bromsgrove. Call that job satisfaction? ‘cause I don’t. Life! Don’t talk to me about Life"
But we do talk to them about Life. Life is our business – Life and Death, that is – and we find we are talking not just a different language, but a different kind of language.
"They’ll want you to measure something, James."
Oops!
"Now just stop juggling for a moment and give me the velocity and angular momentum of that top ball on the right."
Oops!
The Future
So what would the young George Swift want, or the young me, if we were on the Wessex GP training course today, with Jo, a young prospective GP in the Royal Hampshire County Hospital up the road, who spent ten days with me in my practice as a student a few years ago, (and who is also here tonight)?
And at least as important, what would our future patients want, if we cared to ask them? What ideas should the Royal College of General Practitioners be promoting, to restore its hard-won place as the natural focus for innovation and enthusiasm? A place which it lost so tragically by its complicity with the folly of the 1990 contract, and which it urgently needs to regain.
"I say the future is in your hands. You will all have an opportunity to do something new or original. Watch for your opportunity and make it when it comes."
I added a question mark to George Swift’s closing remark in his inaugural lecture, but for those of you who do not know me well I need to make it clear that I am the eternal optimist. I have great confidence in the future of British general practice and of our college.
Being able to make a difference.
But it seems to me that this question of how to keep space in our increasingly buttoned-down world to enable ordinary individuals to flourish and lead rich, rewarding and purposeful lives – to give them their right, in short, to make a difference - is the central challenge of the technological age.
And I’m not so worried about doctors as I am about everybody else - their patients. Doctors on the whole are pretty good at looking after themselves. Not as good as lawyers, who have shrugged off regulation as ducks shrug off pond-water, but we’re not doing too badly. But I have been driven by an anger about the inhuman way so many of my patients have been treated in our supposedly-advanced world, and I think we as doctors, and our college, should use our authority to do something about it for everyone.
There are good arguments, I have given some of them tonight and I have given more in my books and will continue to do so. Others are producing excellent arguments as well. I have no doubt, in fact, that when people in high places condescend to listen for a moment they will find that we have won the argument. But if we all have confidence in the validity of our view of reality, and go on speaking the truth as we find it, and occasionally holding out on matters of principle (a few of us, that is, not so many as to cause chaos) the world will listen, and things could change very fast. Then you and I will have to start arguing like mad to stop them swinging too far the other way.
A new toy
Here is one of the arguments: Our society is experimenting with a new toy - information technology. That is the key factor in this strange assumption that just now, at this particular tick of the great clock of human history, everything is suddenly different.
I have mentioned the Utopian Illusion. If there is a final, Evidence-Based Answer to everything, then it is legitimate for people to think that when anything at all goes wrong it must be somebody’s fault.
But this is an illusion. Things do go wrong. One of the reasons doctors deserve respect in the modern world is that we are one of the few remaining groups who are prepared to accept risk. Even insurers do their best to exclude the people likely to need them, and this is one of the wonderful things about the National Health Service which make it such a great privilege to work in, it does not seek to exclude the needy.
But there is another great irony: one of the best and the most cost-effective interventions in medicine is reassurance. But on the large scale no doctor can give reassurance about anything, and one of the ghastly phenomena of the last year or so has been the way in which we have seen consultant colleagues following drug companies in giving their patients so many warnings and so little direct advice that sorting out the resulting distress and bewilderment has become a major part of the general practice workload.
You CAN be too careful
I believe that the vast majority of GP colleagues still respond as proper doctors, and do what is best for their patients, which often means giving them advice. But in doing so they shoulder the risk which nobody else in our society will take, and it is time they were given back the respect they deserve for that. That accounts for that other mantra of the modern world – ‘you can’t be too careful’. Well you can. That would have been another title for this lecture, in fact, and perhaps a good slogan for the college, "You CAN be too careful" But you only understand this if you take our broad and long term view.
A profound, but hidden, difference
The new toy of information technology produces other distortions that we have hardly begun to think through. Many of them result from the illusion that computers are like human minds. Whether or not computers become like human minds at some point in the future is an open and fascinating debate, but at the moment the difference is profound.
A computer computes very well. That is putting it, to say the least, very mildly.
But a computer can’t juggle.
Nor can that same computer walk around, discriminate a scent, swat a fly, walk a tightrope, fly a plane, and a kite, sing a song, laugh, cry with an audience.
Repair itself…
Grow from a seed…
But a computer can do some of our tricks, and do them much better than us.
It can focus, it can select, it can exclude from attention, much more than we do. But because we have no kind of gauge, we have no instinct for the order of magnitude of the selection, or the proportion which has been excluded, and the picture we see can be hugely more distorted than we comprehend.
A reductio ad absurdum of the computerisation of life
In a very literal sense, the change that is now being imposed on our society, and on medicine, is analogous to it being converted into a computer programme. With all the strengths, and all the weaknesses, that that implies. I believe that we have been so mesmerised by the strengths of the new way of doing things that we have been blind to the weaknesses and the dangers.
But I think the madness that we are seeing in the world today, and this madness is apparent first, as ought to be expected, to front-line generalists who have to balance the whole of life, and last to those on high who have made a virtue of their blinkered thinking, represents a kind of apotheosis. We are on a cusp. Fascinatingly, I think the cusp coincided pretty exactly with the millennium.
Just as we have seen a kind of reductio ad absurdum of the ideals of great pioneering GPs like George Swift, there is a much broader sense in which the whole world is experiencing a reductio ad absurdum of the computerisation of life. I have always thought that British general practice has much to teach the world about generalism, I think we now have much to teach the world about this situation as well. And who better to do this than the Royal College of General Practitioners and its wonderful journal.
To put it very simply, the unprecedented size and complexity of the computers that have become available in the past decade or so has enabled us to attempt to model life in previously inconceivable detail, but always in terms of rigid mathematical rules. And this has revealed for the first time effects which have never been visible before. Just as light appeared always to travel in perfectly straight lines until we developed instruments capable of making observations across intergalactic space – when we quickly confirmed that on that scale the path of light actually curves under the influence of gravity. So we are now seeing, for the first time, that on the large scale life simply doesn’t add up. Again, the theorists got there first, Professor Sir Roger Penrose has been predicting this for years. You can model bits of life very well, that is why specialists are so much less worried by the problem, but try to model the whole of life, which is what we generalists have to deal with, if we are being proper doctors, and the result is madness.
So, the idea that medical knowledge is a finite, definable, deliverable and measurable package is simply wrong. For a grim decade we have been cowed acolytes in a mistaken faith.
But wouldn’t it be wonderful, and wouldn’t it be appropriate, if GPs could lead the way to a more mature understanding of the proper use of technology, as tool rather than master, instead of falling into the trap as giddily as everybody else has done!
The scoring system that I wrote up in the BMJ 15 years ago reduced each of my dependent patient’s medical and social circumstances to a single figure. We could rank them in order. I proposed that the total practice dependency score would be a novel way of comparing workload between practices.
So I do know about this sort of thing, I’ve done it. And this sort of thing is fine, so long as you remain in control, and put human values and human judgement in front of the all-too-easily dominating figures.
The challenge – to maximise the space for human flourishing
So, we should free up life for our successors. They need space, challenge, stimulus. Of course they need rules, of course they need conventions. But the object should be to maximise the space, within the rules, for human flourishing.
The task is difficult because the natural progression of technology calls for more and more uniformity and standardisation. We can see this all around us – from the growing world dominance of the English language, to the almost complete world take-over by the IBM Personal Computer standard. We must win the difficult argument that that there is a huge gulf between this kind of technical matter and individual human activities. Not different things, but different kinds of things.
We must win the argument that the view from on high is not automatically better and more valid, and that the new truths revealed by meta-analysis of enormous trials has not rendered daily human experience, understanding and judgement no longer legitimate as a basis for responsible action. We need small human voices to point out when we are merely making bigger mistakes, with a greater degree of certainty, and imposing them on everyone at once.
It will be difficult, but we are good at achieving difficult things when we think they are important. And the importance here is much more than the mere fact that freedom makes life worth living, the importance is that the alternative doesn’t work. We will always need the free minds and understanding of responsible people at the individual level. That is the meaning of the allegory of Genesis. We have free will, not as a kind of bonus, but because there is no other way the world can work.
Life is not a simultaneous equation, and it doesn’t have one right answer. Mathematical models cannot understand it.
The role of a doctor is to weigh up the whole situation and reach a judgement. We must educate society to respect the difficulty of that kind of task and give doctors, their staff, nurses, teachers, everybody else, the space they need to do their jobs properly. Otherwise doctors, for one, will switch off their common sense and stop bothering to maintain their understanding, and we will have what we deserve - RoboDoc.
Tradition
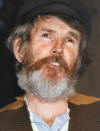
I would like to finish with two more faces. When the darkness came in 1990, I took up amateur dramatics. I have done it ever since..
This is me playing Tevye in Alton Operatic and Dramatic Society’s 1996 production of, Fiddler on the Roof. People found out why I was growing my beard for three months and we sold out all six performances two weeks in advance. This was Tevye’s introduction to the great opening number, Tradition.
A fiddler on the Roof, sounds crazy, no?
But here in our little village of Anatevka, you might say that every one of us is a fiddler on the roof, trying to scratch out a pleasant, simple tune, without breaking his neck. It isn’t easy.
You may ask, why do we stay up there, if it’s so dangerous?
We stay because Anatevka is our home.
And how do we keep our balance?
That I can tell you in one word, Tradition.
Balance. Tradition. I am proud of our traditions in this country. And proud of our famous balance – our gift for compromise. I do not wish to see all this thrown away in the name of change. We must look back, and as we move forward into the excitement of the new, we must keep our balance with the best of the old.
My last patient
Miss Brown was my last patient. She was my last call on my way home on my last afternoon, (two weeks ago now). She lives in an old people’s home just down the road from us, so it fell naturally that way. We sat and chatted, with no pressure of time. I’d never felt like that before. On an impulse I asked her whether she would mind if I had her copy of Axel Munthe’s ‘The Story of San Michele’ that I had been eyeing on her bookshelves. …Never done that before, either, but she couldn’t see to read it any more and it would mean a lot to me to have her copy. "Oh," she said, "that would be lovely"
Ninety seven years old. Taught in a boys boarding school for forty years, now retired for forty years. Already nearly died twice. By chance I’d been on call both times. The first time, after I’d been sitting with the care staff listening to two-minute gaps in her breathing for a long time, she unexpectedly opened her eyes. The first thing she said was, "Oh, I’m so glad it’s you". Now you see why I wanted her book.
She used to walk up the hill to the letterbox opposite our entrance. That was when she still could. We sometimes invited her in, not as often as we meant to, but she came to Christmas dinner with us once. Or was it twice. Last year she just came to tea on the Saturday. And sang hymns from memory, completely happy. I took these pictures then, as you can see.
Apparently she was singing again, the weekend after I’d finished, but she told the staff that she wished I had hung on a bit longer for her. Then, just two mornings after I retired, they found her dead. Cosy in her bed. My last patient.
My only excuse for this story is that it’s true and it somehow seemed a good way of finishing. You know, the importance of humanity, and all that.
We went to her funeral last week. There were half a dozen distinguished-looking grey-haired men there who turned out to have been in her boarding-house when they were little boys. Wonderful singing. One of them doing a brilliant tenor line from memory. Her surrogate sons, and you could see a lot of her in them, fifty years later.
I should like to thank the people who have added so much to my picture of George Swift, especially Philip Carter, Chris Brill, David Morrell and James McCormick, and to the many people who have helped me give this lecture such coherence as it has achieved, especially my Lesley, and Judith Hepper, both teachers I have to say.
And I thank you all, once again, and very sincerely, for coming to listen – to the juggler.